| |
Post-operative residual curarization (PORC) - A Big Issue for Patients’ Safety |
| |
 |
| |
Definition |
| |
PORC is an abbreviation for postoperative residual curarization, identified by instrumental signs (TOF Ratio <0.9 -1.0) and clinical signs such as: |
| |
 |
Evident muscle fatigue or 'fade' |
|
 |
Attenuation of the hypoxic reflex |
|
 |
Pharyngolaryngeal dysfunction with loss of airway patency and the risk of "aspiration" |
|
 |
Reduction of the cough reflex |
| |
Incidence |
| |
| Study |
Pancuronium |
Atracurium |
Vecuronium |
Rocuronium |
| Bevan et al |
36% |
4% |
9% |
|
| Hayes et al |
|
52% |
64% |
39% |
| Baillard et al |
|
|
42% |
|
| Kim et al |
|
|
25% |
15% |
| Murphy et al |
40% |
|
|
5.9% |
|
| |
Adverse effects of residual neuromuscular block |
| |
Volunteer studies |
| |
 |
Impaired pharyngeal function |
 |
Increased risk of aspiration |
 |
Upper airway obstruction |
 |
Impaired hypoxic ventilatory drive |
 |
Profound symptoms of muscle weakness |
|
| |
Clinical studies in surgical patients |
| |
 |
Delays in meeting PACU discharge criteria and achieving actual discharge |
 |
Symptoms and signs of profound muscle weakness |
 |
Increased risk of postoperative hypoxemia |
 |
Prolonged postoperative intubation times (cardiac surgical patients) |
 |
Increased risk of postoperative respiratory complications |
|
| |
Assessment of residual neuromuscular block |
| |
Visual and tactile evaluation (for surface muscles): Subjective method and therefore dependent on the individual assessment. |
| |
Among the various clinical criteria, there are some proved unreliable (tongue protrusion, eye opening, normal or near normal vital capacity, inspiratory pressure < -25 cm H2O, arm raised toward the opposite shoulder), others not very reliable (head lift test, holding hand for 5 seconds, lifting leg for 5 seconds, maximum inspiratory pressure > - 50 cmH2O), and finally the only one that seems pretty reliable, the tongue depressor test, which seems to correspond to a value of TOF> 0.8 -0.9. |
| |
Clinical tests used to assess adequacy of reversal for neuromuscolar blockade: |
| |
| Induction of muscle relaxation |
| Reduction or disappearance of the respiratory movements |
| Fasciculations (succinylcholine)< |
| Easy extension of the head |
| Easy positive pressure mask ventilation |
| mouth opening |
| Easy tracheal intubation |
| Absence of cough during intubation |
| Maintenance of muscle relaxation |
| Relaxation of the abdominal muscles |
| If partial paralysis: maladaptation to mechanical ventilation, diaphragmatic movements,
increased peripheral muscle tone, contraction of frontal muscles, eyelid reflex
|
| Recovery of muscle relaxation: Testing of awakening |
| Ability to lift the eyelids |
| Ability to protrude the tongue |
| Ability to cough |
| Ability to shake hands |
| Ability to keep an arm raised |
| Ability to lift head |
| Vital capacity greater than 15 ml / kg |
| Inspiratory force of at least -25 cmH20 |
| Tongue-depressor test: ability to squeeze an object between the teeth, resisting the removal |
|
| |
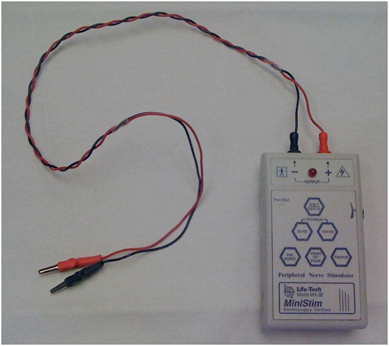
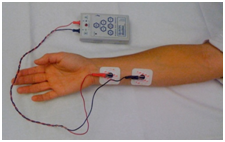
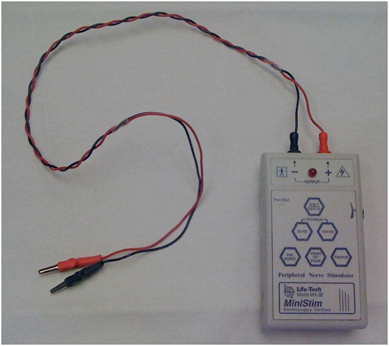
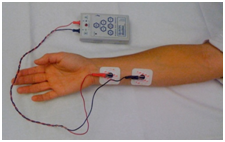
Standard peripheral nerve stimulator |
| |
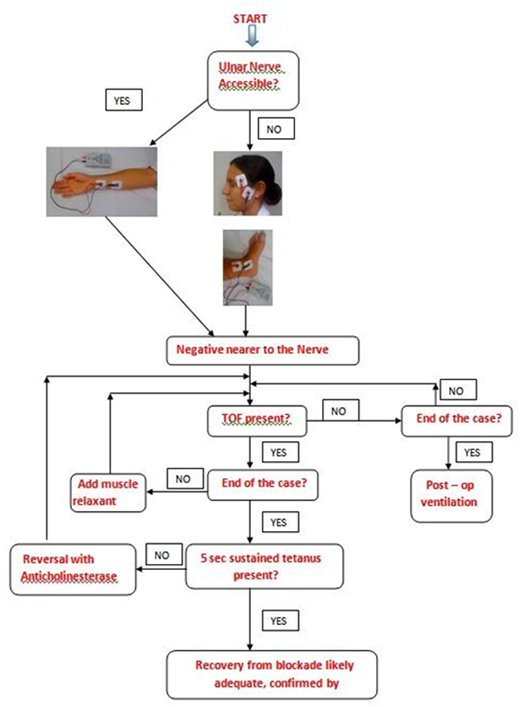
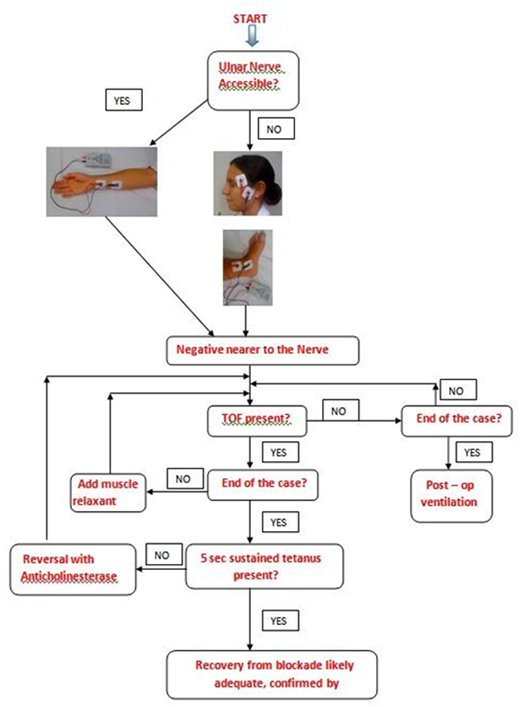
The ulnar nerve at the wrist is the most popular site for neurostimulation, and the response at the adductor pollicis is observed. The facial nerve is also frequently used as a monitoring/stimulation site, and contraction of the muscles around the eye evaluated. |
| |
|
 |
 |
| |
 |
| |
 |
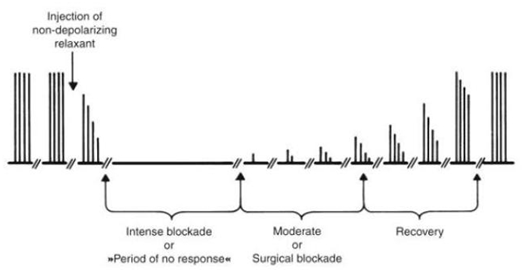
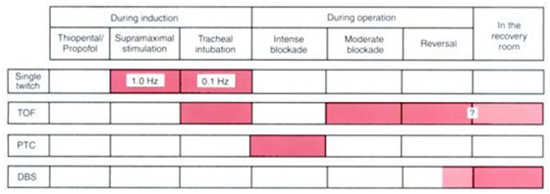
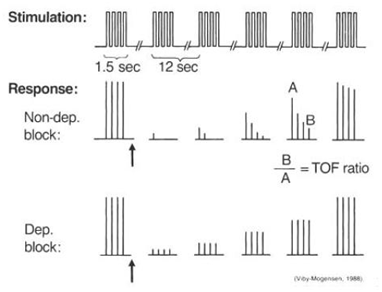
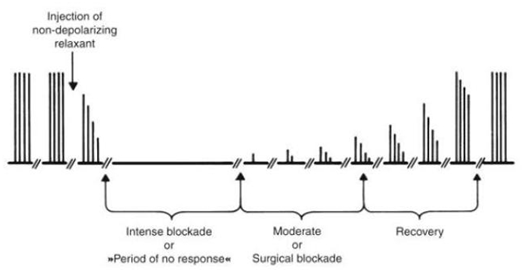
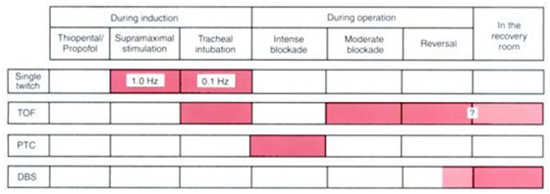
Single twitch: In the single-twitch mode of stimulation, single supramaximal electrical stimuli are applied to a peripheral motor nerve at frequencies ranging from 1.0 Hz (once every second) to 0.1Hz (once every 10 seconds) Twitch height will begin to decrease when 75% of nicotinic acetylcholine receptors are blocked and will disappear when 90-95% of the receptors are occupied. |
 |
 |
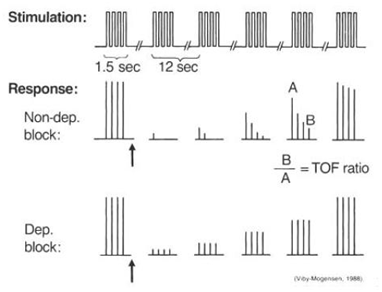
TOF: TOF stimulation is the most frequently used pattern of neurostimulation in the perioperative setting. In TOF nerve stimulation, introduced by Ali and associates during the early 1970s, four supramaximal stimuli are given every 0.5 seconds (2 Hz) The TOF count is simple to perform and does not require a control twitch height. When 70-75% of the nicotinic acetylcholine receptors are blocked, the forth response (T4) is decreased. The T3, T2, And T1 responses are abolished when 85%, 85-90%, and 90-98% of the nicotinic acetylcholine receptors are occupied, respectively. |
 |
 |
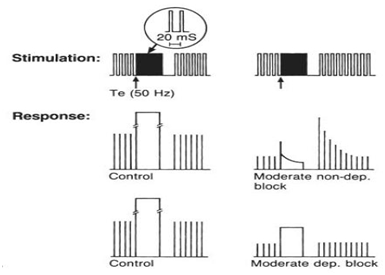
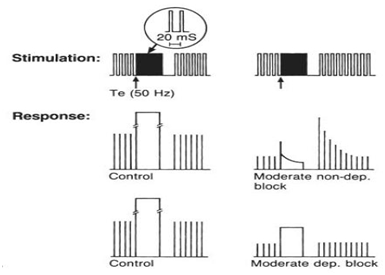
Tetanic stimulation and post-tetanic count: stimulation of motor nerves at frequencies >30 Hz results in fusion of twitch responses and a sustained muscle contraction. Fade (decrease in muscle response to rapid stimulation) is observed during tetanic stimulation when more than 70-75% of the nicotinic acetylcholine receptors are blocked.
The degree of fade can be used to estimate the intensity of neuromuscular blockade. When a single twitch stimulus is applied within 2 min of a tetanic stimulus, an enhanced response occurs as a result of posttetanic potentiation. A post-tetanic count is performed by applying supramaximal stimuli once every second following a 5-s 50 Hz tetanic stimulus. The post-tetanic count can be used to assess deep neuromuscular blockade and to estimate time to recover twitches when no response to TOF stimulation is present. |
 |
 |
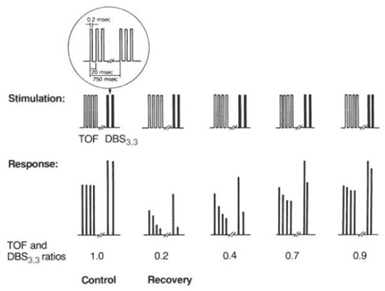
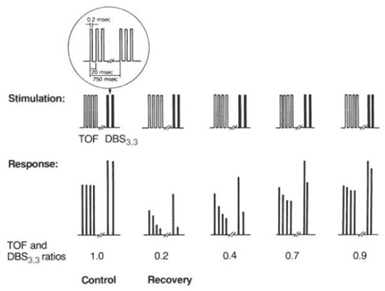
Double-burst stimulation (DBS): DBS involves the application of 2 short bursts of tetanic stimuli (50 Hz) separated by a 750 ms interval. Each burst consist of a series of 3 and 2 impulses (DBS3,2) or 3 and 3 impulses (DBS3,3). DBS was developed to allow clinicians to more accurately assess small degrees of residual paresis using visual or tactile observations.
Pattern of electrical stimulation and evoked muscle responses to TOF nerve stimulation and double-burst nerve stimulation: |
 |
|
| |
Clinical uses of stimulation |
| |
Nerve stimulation in clinical anesthesia is usually synonymous with TOF nerve stimulation. Therefore, the recorded response to this form of stimulation is used to explain how to evaluate the degree of neuromuscular blockade during clinical anesthesia. |
| |
 |
| |
Which modes of nerve stimulation can be used at various periperative times |
| |
 |
| |
Quantitative neuromuscular monitoring |
| |
Quantitative neuromuscular monitoring was developed in order to allow clinicians to accurately measure single twitch height and TOF ratio values. Three methods of recording evoked responses are available: |
| |
 |
Mechanomyography: mechanomyography measures the mechanical force of a muscle contraction. Isometric contraction of the adductor pollicis is quantified following ulnar nerve stimulation. |
| |
However, since the equipment is bulky and difficult to set up and use, mechanomyography is rarely used in clinical practice. |
 |
Electromyography (EMG): EMG measures the electrical activity (compound muscle action potentials) of the stimulated muscle. Typically, EMG responses are measured with electrodes at the thenar eminence, the hypothenar eminence, or the first dorsal interosseous muscles of the hand. |
| |
EMG is rarely used in the operating room setting. |
 |
Acceleromyography: mechanomyography and electromyography are utilized primarily as research tools. Acceleromyography technology was developed for routine clinical use in the operating room, PACU, and ICU. |
| |
Acceleromyography is based on Newton’s second law which states that force = mass x acceleration. If mass is constant, force can be calculated by measuring acceleration. Acceleration of the stimulated muscle is quantified using a small piezoelectric crystal embedded in a transducer. A small electrical signal is generated in the transducer during movement of a muscle, which is amplified and displayed on the device. Since no preload is required on the stimulated muscle, additional monitoring sites can be used (muscles surrounding the eyes). |
|
| |
Algorithm illustrating the logic for the use of a PNS during the course of Anaesthesia |
| |
 |
| |
Methods to reduce the risks of residual neuromuscular blockade |
| |
 |
Avoidance of long-acting NMBAs |
 |
Use of routine neuromuscular monitoring in the operating room |
 |
Acceleromyography monitoring during the surgical procedure and prior to tracheal extubation may have a beneficial impact on the incidence of residual paresis. |
 |
Avoidance of total twitch suppression(Reversal of neuromuscular blockade should not be attempted until spontaneous recovery of neuromuscular function has occurred (at least 1 response to TOF stimulation). The risk of intense neuromuscular block at the conclusion of the surgical procedure is increased if a TOF count of 0 is maintained intraoperatively. Fortunately, profound muscle relaxation is rarely required in the operating room. A TOF count of 0 should be maintained during a surgical procedure only if patient movement or coughing could result in serious injury (i.e., during ophthalmic surgery on an open globe or during procedures on patients with critically elevated intracranial pressure). Adequate surgical relaxation (abdominal surgery) is usually present at a TOF count of 1-2.) |
 |
Routine reversal of NMBAs’ |
 |
Reversal of neuromuscular blockade at a TOF count of 2-3 |
 |
Early antagonism of neuromuscular blockade
(Since full reversal of more intense levels of neuromuscular block may require up to 20-30 min, anticholinesterases should be used at least 15-30 before the anticipated time of tracheal extubation. Antagonism of NMBAs should be initiated when muscle relaxation is no longer needed instead of at the conclusion of skin closure) |
|
| |
Note |
| |
| It is difficult, and often impossible, by clinical evaluation of recovery of neuromuscular function, to exclude with certainty clinically significant residual curarization. |
|
| |
| Absence of tactile fade in the response to TOF stimulation, tetanic stimulation and DBS does not exclude significant residual block |
|
| |
Ref: |
| |
1. Post-Operative Residual Curarization (PORC): A Big Issue for Patients’ Safety A. Castagnoli, M. Adversi, G. Innocenti, G.F. Di Nino and R.M. Melotti Anesthesiology and Intensive Care, S. Orsola-Malpighi Hospital, University of Bologna,Italy. |
| |
2. Residual neuromuscular blockade: incidence, assessment, and relevance in the postoperative period. G. S. MURPHY, MINERVA ANESTESIOL 2006;72:97-109 |
| |
3. Neuromuscular Monitoring - Jørgen Viby-Mogensen |
| |
4. Neuromuscular monitoring and postoperative residual curarization: a meta-analysis British Journal of Anaesthesia 98 (3): 302–16 (2007) |
| |
5. Postoperative Residual Curarization: Clinical Observation in the Post-anesthesia Care Unit. Chang Gung Med J Vol. 31 No. 4 July-August 2008 |
| |
6. Postoperative residual curarization from intermediate-acting neuromuscular blocking agents delays recovery room discharge. Br. J. Anaesth. (2010) 105 (3): 304-309. |
| |
7. Bevan DR, Smith CE, Donati F. Postoperative neuromuscular blockade: a comparison between atracurium, vecuronium, and pancuronium. Anesthesiology 1988;69:272-6. |
| |
8. Hayes AH, Mirakhur RK, Breslin DS, Reid JE, McCourt KC. Postoperative residual block after intermediateacting neuromuscular blocking drugs. Anaesthesia 2001;56:312-8. |
| |
9. Baillard C, Gehan G, Reboul-Marty J, Larmignat P, Samama CM, Cupa M. Residual curarization in the recovery room after vecuronium. Br J Anaesth 2000;84:394-5. |
| |
10. Debaene B, Plaud B, Dilly MP, Donati F. Residual paralysis in the PACU after a single intubating dose of nondepolarizing muscle relaxant with an intermediate duration of action. Anesthesiology 2003;98:1042-8. |
| |
11. Kim KS, Lew SH, Cho HY, Cheong MA. Residual paralysis induced by either vecuronium or rocuronium after reversal with pyridostigmine. Anesth Analg 2002;95:1656-60. |
| |
12. Murphy GS, Szokol JW, Franklin M, Marymont JH, Avram MJ, Vender JS. Postanesthesia care unit recovery times and neuromuscular blocking drugs: a prospective study of orthopedic surgical patients randomized to receive pancuronium or rocuronium. Anesth Analg 2004;98:193-200. |