| |
KETAMINE IS GOING TO BE OUT OF REACH! |
| |
The UN Commission on Narcotic Drugs will hold its 58th meeting in Vienna, starting on 9th March, and there will be an attempt to place further international restrictions on the distribution and use of ketamine. |
| |
 |
| |
Fact Sheet on the Proposal to Discuss International Scheduling of Ketamine at the 58th CND |
| |
Introduction |
| |
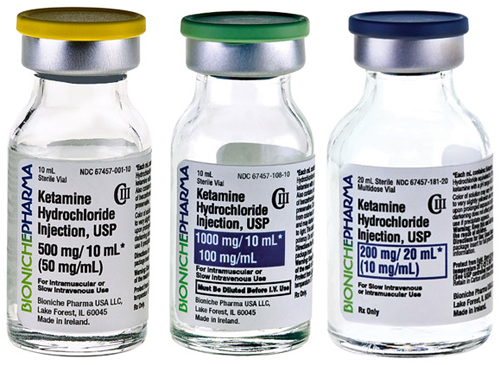
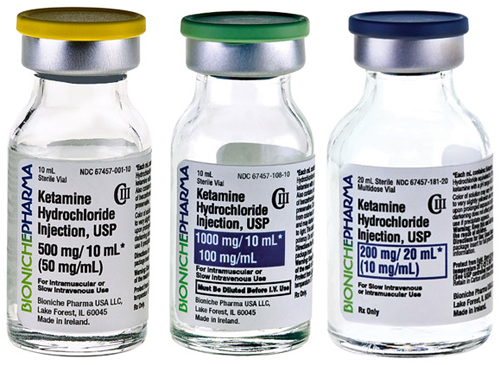
Ketamine is an essential medicine used for anaesthesia. It is the only available anaesthetic for essential surgery in most rural areas of developing countries, home to more than 2 billion of the world’s people. Scheduling ketamine will leave these populations with no alternative anaesthesia for essential surgery, and will further deepen the already acute crisis of global surgery. |
| |
The Commission on Narcotic Drugs, 58th Session, has been asked to review a proposal to place ketamine in Schedule I of the 1971 Convention (E/CN.7/2015/7 and E/CN.7/2015/81). As per the terms of the 1971 Convention on Psychotropic Substances, the WHO Expert Committee on Drug Dependence (ECDD) critically evaluated ketamine in 2006, 2012 and 2014. Based on accumulated evidence and data on non-medical use, diversion and trafficking, and evidence of ketamine’s therapeutic value, the ECDD does not recommend that the CND place ketamine under international control. |
| |
A wide range of national and international civil society organizations, have voiced concern about the proposal. This basic fact sheet provides compelling legal, medical and social arguments against placing ketamine in any schedule of the 1971 Convention. Section I covers definitions and substantive issues; Section II, procedural issues. |
| |
Section I: substantive issues |
| |
What is ketamine? And how important is ketamine in human and veterinary medicine? |
| |
Ketamine is a medication used as an anaesthetic in human and veterinary medicine. Because it is readily available, easy to use and inexpensive, ketamine is one of the most commonly used anaesthetic agents in developing countries. It is also used recreationally in some countries as a “party drug.” The World Health Organization considers ketamine an “essential medicine” and does not recommend scheduling it under the international substance control conventions. Regarding essential surgery, a WHO document states that ketamine must be accessible in all facilities where anaesthesia is needed, in order to ensure safe and affordable surgical care. |
| |
Ketamine is also the primary anaesthetic used in veterinary practice. Scheduling ketamine would restrict access and lead to losses in the agricultural economy. |
| |
How harmful is non-medical use of ketamine? |
| |
The non-medical use of ketamine has limited harmful effects. After a notification by China suggesting that ketamine be placed in Schedule I of the 1971 Convention, the ECDD critically reviewed it again in 2014. The ECDD considered peer reviewed reports and data regarding ketamine’s recreational use in some urban areas, the likelihood of its potential to cause dependence if used non-medically, epidemiological evidence of morbidity and mortality rates, as well as records of police seizures of illicit supplies. After weighing all the reports, this international expert panel concluded that “ketamine abuse currently does not appear to pose a sufficient public health risk of global scale to warrant scheduling” and recommended that “ketamine not be placed under international control at this time”. |
| |
Why does the WHO ECDD recommend against international control of ketamine? |
| |
Further to the above, the ECDD considered evidence submitted from all over the world that ketamine is widely used as an anaesthetic in human and veterinary medicine, especially in low- and middle-income countries, as well as in emergency situations. Ketamine is easily administered by trained providers. Compared to anaesthetic gases, which require costly equipment and appropriately trained specialists, it is inexpensive and safe to administer. Since many countries have no appropriate or affordable alternatives, scheduling ketamine would force patients in those regions to forego lifesaving essential surgery, further compromising realization of the health-related Millennium Development Goals. |
| |
What would be the public health impact of a placing ketamine in Schedule I? |
| |
Under the terms of the 1971 Convention, medicines in Schedule I have “very limited medical usefulness”. Parties to the Convention are obliged to prohibit any medical use of a Schedule I substance except by "persons directly under control of the government,” and even use for and by those persons is very restricted (Art. 7). Providers in non-government institutions and clinicians in remote areas, especially in resource poor settings, will be unable to use ketamine if it is placed in Schedule I. |
| |
The control stipulated for Schedule I substances would be very inappropriate for ketamine, given its critical use in developing countries and in zones of armed conflict where high-tech resources, labs, operating rooms etc. are unavailable. |
| |
People living in rural areas of low-resource countries will not have access to essential surgery if ketamine is less available, or completely unavailable. International restrictions could potentially affect the health of an estimated 2 billion or more people, living mainly in Africa, Asia and Latin-America. |
| |
What about placing ketamine in another schedule? |
| |
The WHO ECDD did not recommend placing ketamine in any schedule. Hypothetically, however, placing ketamine in any other schedule would also limit its availability and accessibility, both of which are mandatory criteria for essential medicines. The cumulative evidence from over fifty years of international drug control shows that restrictive regulatory requirements imposed by scheduling essential medicines create costly burdens for low resource countries. Strict scheduling requirements result in decreased clinical use or abandonment altogether. In the words of the Convention, “the use of psychotropic substances for medical and scientific purposes is indispensable and […] their availability for such purposes should not be unduly restricted". |
| |
Is there a way to limit misuse and diversion of ketamine? |
| |
Ketamine is difficult to synthesize and does not lend itself to large scale illicit manufacture. UNODC reports that China is the source of much of the world's illicitly consumed ketamine, which has either been diverted from legitimate pharmaceutical manufacture, or illicitly produced and then domestically or internationally trafficked. The NGOs endorsing this letter call on the government of China to take the necessary steps to prevent the diversion, illicit manufacture and export of ketamine beyond its national frontiers, rather than to promote international scheduling. |
| |
Section II. Procedural Issues |
| |
Can the 58th CND decide to schedule ketamine under the 1971 Convention? |
| |
Article 2, paragraph 5, of the 1971 Convention states that the Commission may add a substance to a schedule only following an explicit WHO recommendation to do so. As per the official Commentary to the Convention (p. 46): “the phrase ‘recommendations on control measures,’ means ‘recommendations on the schedule in which the substance in question should be placed”. Since the WHO recommended in 2014 that ketamine not be placed in any of the schedules, there is no extant recommendation that could legally serve as the basis of a scheduling decision by the CND. |
| |
Under these circumstances, placing a scheduling proposal for ketamine on the CND agenda would contravene the terms of the 1971 Convention. |
| |
Can the CND disregard a WHO recommendation to schedule or not to schedule a substance? |
| |
No. As discussed above, the CND can consider scheduling a substance only if the WHO has recommended that the substance be placed in a schedule. In such a case, State Parties can select a schedule other than the schedule recommended by WHO based on relevant economic, social, administrative or other factors. Article 2, paragraph 5 of the 1971 Convention states, however, that the WHO’s medical and scientific determination is final. |
| |
Notifications by Parties to the Convention are not a basis for CND decision making about including substances in the treaty schedules. Regarding medical and scientific aspects, these notifications can only serve to inform other Parties, the CND, and WHO for the purposes of their evaluative process. |
| |
Following notifications by State Parties, CND can only decide to take provisional control measures, while awaiting the recommendation of the WHO. But in the case of ketamine, since WHO already issued its recommendation, the option of a provisional control measure no longer applies. |
| |
How does the continuing pressure on WHO affect its ability to fulfil its mandate under the international substance control conventions? |
| |
Following requests from China, the International Narcotics Control Board and others, the World Health Organization’s ECDD reviewed ketamine in 2006, 2012 and 2014, each time concluding that scheduling is not warranted. Ketamine’s medical importance has been well documented, while evidence of its harmful properties is limited. Performing additional reviews in the near future would be inefficient and costly. WHO is also under pressure to evaluate a large number of New Psychoactive Substances (NPS) and to re-evaluate several scheduled substances it had evaluated in the distant past. WHO’s substance evaluation mandate gives it a critical role in safeguarding global health. The ability to fulfil this mandate is dependent on the States Parties and UN bodies abiding by the conventions – in this case, following the WHO’s expert recommendations. |
| |
Note: |
| |
China, a major producer of ketamine, is understood to be concerned by its abuse and it has the support of a number of other countries, including Russia. It will need backing from two-thirds of the 53 member states. The UK has said it will abstain on the vote, which is tantamount to a no. |
| |
Campaigners argue the proposal should not have been brought at all. “Legally, WHO [World Health Organisation] must consent before the commission can add any drug to schedule 1,” said Amir Attaran, law professor at the University of Ottawa in Canada. “WHO has thrice come out unequivocally against scheduling ketamine.” |
| |
He argues that the UN Office on Drugs and Crime, the secretariat of the Commission on Narcotic Drugs, should not have put the draft resolution forward for discussion. |
| |
“China has been pushing for a long time,” said Willem Scholten, an independent consultant in controlled medicines in the Netherlands who was secretary of WHO’s expert committee on drug dependence until two years ago. Beijing first put it forward in 2005 and it was reviewed again in 2012 and in 2014 – each time WHO advised against it because of the potential impact on health in the developing world. |
| |
When the resolution is debated by the commission, it is understood that the scientific and medical opinion of the WHO will not be challenged. The argument then will centre on the experiences of crime and drug abuse put forward by the individual member states. |
| |
SOURCE: |
| |
The Gaudian and Message from AAGBI President, Dr Andrew Hartle |